Do You Have Any of These Telltale Signs of Plaque Psoriasis?
Published on
8 minute read
Plaque psoriasis is a common autoimmune disease. Millions suffer as it makes the immune system attack the skin cells. This leads to fast skin cell growth, causing scaly patches. These patches might cover small or large areas, causing discomfort.
It’s vital to know the signs of psoriasis, its triggers, and the types and levels of severity. Recognizing flare-ups and remission phases is essential. Thankfully, psoriasis isn’t contagious.
Those with plaque psoriasis experience cycles of clear skin and challenging flare-ups. The symptoms don’t mean the disease can spread by touch. Getting to know this condition means understanding all aspects, from visible signs to the underlying cell behavior.
Key Takeaways
- Plaque psoriasis is an autoimmune condition leading to rapid skin cell growth and scaly patches.
- Psoriasis shows cycles of flare-ups and remission, signaling the importance of ongoing management.
- Understanding psoriasis symptoms and signs is vital for identification and treatment.
- Despite its appearance, psoriasis is not contagious, allowing individuals to maintain regular social interactions.
- Being informed about psoriasis causes, types, and severity aids in better healthcare decisions.
Understanding Plaque Psoriasis and Its Impact on Your Health
Managing plaque psoriasis starts by understanding it is an autoimmune disease. It’s a complicated skin condition. It changes the lives of those who have it. This requires knowing how to treat psoriasis and understanding its cycles.
The Autoimmune Origin of Plaque Psoriasis
The immune system of someone with plaque psoriasis attacks healthy skin cells by mistake. This leads to skin cells growing too fast. It’s this wrong response that causes psoriasis, making treatment and management challenging.
Cycles of Psoriasis Flare-ups and Remission
Plaque psoriasis involves cycles of bad flare-ups and quiet times of remission. Knowing these cycles helps in planning long-term treatment. This keeps skin healthy and lessens its impact on daily activities.
Not Contagious: Dispelling Common Myths About Psoriasis
There are wrong ideas about plaque psoriasis being catchy, isolating patients. It’s crucial to share that it’s not contagious. Doing so builds community support and improves life for those affected.
| Psoriasis Phase | Skin Appearance | Impact on Quality of Life |
|---|---|---|
| Active Flare-up | Red, scaly plaques | Increased discomfort and potential social withdrawal |
| Remission | Possible residual discoloration | Improvement in overall wellbeing and everyday function |
Recognizing the Symptoms: More Than Just Skin Deep
Identifying psoriasis symptoms goes beyond seeing skin scaliness. Psoriasis affects the body in more ways, impacting overall health deeply. It brings about a strong psoriasis itching sensation. This can make someone want to scratch, hurting their skin more.

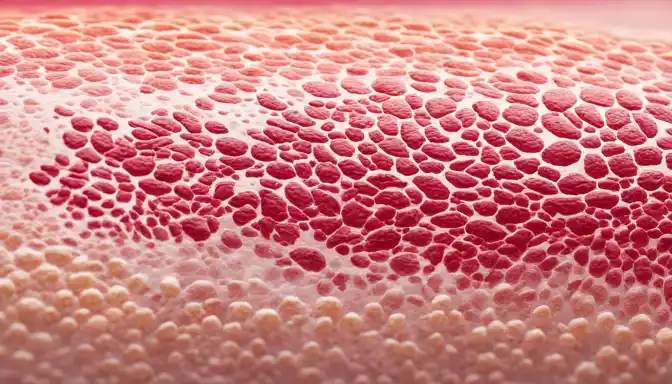
Psoriasis scaling involves extra skin cells piling up, creating silvery-white scales. These usually appear on elbows, knees, and the scalp. These scales show deep inflammation beneath them. Red skin areas, pointing to psoriasis inflammation, result from the body trying to fix the rapid skin cell production.
Psoriasis can also show as small, red dots, especially after strep infections. Inverse psoriasis leads to red, glossy patches in body folds, differing from the thick plaques of plaque psoriasis. Scalp psoriasis might look like severe dandruff but causes more itching and can even cause hair loss if untreated.
Sometimes, psoriasis symptoms include non-infectious pus-filled pustules in pustular psoriasis. It’s key to understand these are not just surface issues. They signal a deeper, chronic condition needing medical care.
Plaque Psoriasis: Identifying Characteristic Skin Manifestations
Plaque psoriasis is more than just an inconvenience. It shows in various types and severity levels on the skin. It’s key to understand these changes for the right diagnosis and treatment.
The Appearance of Silver, Scaly Patches
Silver, scaly patches are a main sign of plaque psoriasis. These patches usually appear on the elbows, knees, and scalp. They are important for identifying this condition.
Red Patches and Small, Red Dots
Besides scaly patches, some people get red areas or tiny red dots. These signs show different severity levels of psoriasis. It’s important to look closely to tell them apart from other conditions.
Distinguishing Between Psoriasis and Other Skin Conditions
Eczema and dermatitis have similar symptoms to psoriasis but don’t have the thick, silver scales. Spotting these differences is crucial. It shows why a professional diagnosis is needed for skin health.
| Psoriasis Symptom | Appearance | Common Locations | Key Differentiators |
|---|---|---|---|
| Silver, Scaly Patches | Thick, silver-white scales; | Elbows, Knees, Scalp | Extensive scaling, well-defined edges |
| Red Patches | Smooth, red lesions; | Body Folds (Inverse Psoriasis) | Well-defined, often shiny |
| Small, Red Dots | Tiny, drop-like dots; | Trunk and Limbs (Guttate Psoriasis) | Often appear after a strep infection |
| Dermatitis/Eczema | Red, itchy rash; | Varies greatly | More diffuse borders, intense itch |
Psoriasis Beyond the Skin: Additional Physical Signs
Psoriasis is known for its skin plaques but its effects go deeper. Joint pain and symptoms of autoimmune issues can be a part of it too. This is why looking at the whole picture is key in treatment.
Joint Pain and Psoriatic Arthritis
For those with psoriasis, psoriatic arthritis is a big concern. It causes joint inflammation, leading to pain and stiffness. Just like psoriasis affects the skin, this condition targets the joints.
Nail Changes and Their Significance in Diagnosis
Nail changes, like pitting or detachment, could point to psoriasis. These signs are important for diagnosing. They might also hint at psoriatic arthritis before any joint pain starts.

The Physical Discomfort of Itching and Burning Sensations
Living with psoriasis can bring lots of discomforts, like itching and burning. Handling these symptoms is crucial in psoriasis treatment.
| Symptom | Physical Manifestation | Impact on Daily Life |
|---|---|---|
| Skin Plaques | Silvery scales, red patches | Social discomfort, clothing choice restrictions |
| Joint Pain | Swelling, stiffness in joints | Limited mobility, difficulty in daily activities |
| Nail Changes | Pitting, discoloration | Self-consciousness, potential early sign of psoriatic arthritis |
| Itching/Burning | Dry, cracked skin prone to bleeding | Constant discomfort, sleep interruptions |
Addressing Psoriasis: When to Seek Medical Advice
Dealing with psoriasis is tough. Getting medical advice early is crucial for managing this condition. Many psoriasis medications can help control symptoms and prevent flare-ups. Since treatments vary, it’s essential to see a healthcare professional. They can create a treatment plan that fits you perfectly. Remember, what works for one person might not work for another. This is why expert advice is so valuable.
Trying psoriasis natural remedies? Get professional advice to ensure these fit with other treatments. Joining psoriasis support groups can also help. You’ll get emotional support and learn practical tips from others with psoriasis.
When symptoms get worse, explore all treatment options. Psoriasis light therapy might be recommended for reducing plaque symptoms. Psoriasis topical treatments provide quick relief and are usually the first choice.
Consider holistic options like aloe vera, turmeric, and omega-3s for their anti-inflammatory effects. Their success varies, so checking with a doctor is key. As you work towards better health, leaning on psoriasis support from health teams and community groups is vital for your mental and physical wellness.
- Consult with healthcare providers for a personalized medication plan
- Evaluate the effectiveness of topical creams and ointments for targeted treatment
- Determine if light therapy could be a beneficial addition to your treatment regimen
- Investigate natural remedies and discuss them with your doctor to safely incorporate them
- Seek out support networks for additional guidance and emotional resilience
Deciding to seek medical advice for psoriasis is about wanting a better life. You aim for symptom relief and control over the condition. By doing this, you can create a comprehensive plan that reduces the risk of complications like psoriatic arthritis. This leads to an overall better quality of life.
Conclusion
In wrapping up the dialogue on plaque psoriasis, effective management relies on early recognition, medical advice, and lifestyle changes. A psoriasis diet that reduces inflammation helps. Making lifestyle changes and using the right skincare can improve life quality for those with this condition. By adopting these strategies, people can lower the number and severity of flare-ups and keep their skin healthier.
Managing stress is also key in controlling psoriasis symptoms. Techniques like mindfulness and regular exercise help in achieving a better emotional balance. This can help lessen skin reactions. Such methods help the body handle stress that could cause psoriasis flare-ups, leading to a more resilient lifestyle.
Living with plaque psoriasis involves dealing with its emotional impact, which can vary greatly. Recognizing the emotional aspects is crucial in a full treatment plan. Therefore, the journey to remission includes both clinical and personal attention. Integrating physical and emotional care helps alleviate symptoms and strengthens emotional well-being. This brings balance and hope to those struggling with this skin condition.
FAQ
What are the common signs of plaque psoriasis?
Plaque psoriasis signs include red, inflamed skin with silver scales. You might see this on the elbows, knees, and scalp. The severity ranges from small to extensive areas. Symptoms can come and go, sometimes even going into remission.
How does plaque psoriasis affect my health?
This autoimmune disease causes cycles of flare-ups and remission. It affects skin and joints but isn’t contagious. It can lead to psoriatic arthritis, causing joint pain and stiffness. This impacts overall health and quality of life.
Can plaque psoriasis manifest in ways other than scaly skin patches?
Yes, it can. Plaque psoriasis may cause small red dots or shiny patches in body folds. It can look like dandruff on the scalp and change how nails look. Some folks get joint pain or psoriatic arthritis too.
How can I differentiate between plaque psoriasis and other skin conditions?
Look for silver, scaly patches and well-defined red lesions on places like the scalp, elbows, and knees. Unlike eczema or dermatitis, psoriasis plaques are thicker with a silvery shine.
What physical discomforts are associated with psoriasis beyond the visual symptoms?
Psoriasis can make your skin itch and burn. It can also cause dry, cracked skin that might bleed. And when it turns into psoriatic arthritis, it brings pain and stiffness.
What steps should I take if I suspect I have psoriasis?
If you think you have psoriasis, see a doctor for a proper diagnosis and treatment plan. They can suggest medications, topical treatments, light therapy, or natural remedies to manage symptoms.
How can making lifestyle changes help manage psoriasis?
Making lifestyle changes can really help. Eat well, manage stress, and care for your skin properly. These steps can reduce flare-ups, make your skin healthier, and improve your life overall.